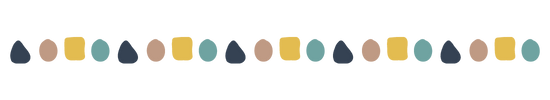
In neurodivergence, co-occurring conditions refer to neurodevelopmental, physical, and mental health conditions that can show up in the same neurodivergent person. Co-occurring conditions form part of the wider category of co-occurrence, which also refers to how certain neurodivergent traits tend to appear together.
Understanding co-occurrences is a vital part of the neurodivergent discovery journey, because it explains how different aspects of neurodivergence affect your brain and body throughout your lifetime. Co-occurring conditions and traits are very common in neurodivergence, and this knowledge can take a lot of guesswork out of your health journey throughout your life.
Patterns of co-occurrence in neurodivergence extend beyond neurodevelopmental differences: neurodivergent conditions are often co-occurrent with various physical and mental health conditions and experiences. Understanding co-occurrence is vital because it helps explain how different aspects of neurodivergence connect, leading to better self-understanding and more effective support. While traditional healthcare often treats conditions separately, recognising these natural connections can transform how you advocate for your needs and access appropriate care.
There are many overlapping traits and symptoms in neurodivergent conditions, so much so that some experts say that in the next decades, many of them will be merged into one group. It is possible to get multiple diagnoses because of this. 9
Table of Contents[Hide][Show]
Co-occurrence or comorbidity?
We use the term co-occurrence across our website and resources because we have a trait-based look on neurodivergence, which includes positive and neutral traits that are not symptoms in the medical sense. In medical settings, you’re more likely to hear the word comorbidity as the focus of health care practitioners is to identify and alleviate health problems.
We talk about co-occurrence to cover a wide range of things that show up in and around neurodivergence. Co-morbidity is a co-occurrence. Medical conditions showing up simultaneously with neurodevelopmental conditions. However, co-occurrence can also mean symptom overlap
The four types of co-occurrence in neurodivergence
Neurodivergence shows up in every area and facet of life. The differences compared to neurotypical physiology permeate a person’s physical and mental health. So when we talk about co-occurrence in neurodivergence, this can mean the following categories:
- If you’re experiencing the traits of one neurodivergent condition, you’re more likely to also find you have traits of other neurodivergent conditions — regardless of whether you hit the full diagnostic criteria of those conditions.
- If you’re neurodivergent, that has profound impacts on your physical health. There’s a whole host of physical conditions that are more likely to show up for neurodivergent people than for the neurologically typical population.
- Neurodivergence also affects mental health in multiple ways, meaning there’s a whole range of mental health experiences that tend to show up more often for neurodivergent folks.
- Finally, there are specific neurodivergent trait combinations that tend to go together – certain neurodivergent traits make the emergence of other neurodivergent traits more likely.
1. Co-occurrence within neurodivergence
When you’re neurodivergent, it’s extremely common to experience multiple forms of neurodivergence together. This pattern of co-occurrence means that having one form of neurodivergence significantly increases the likelihood of having others. As the most significant example that not nearly enough people are aware of, between 30-80% of autistic people also have significant ADHD traits, while 20-50% of people with ADHD meet the criteria for autism 7.
2. Co-occurrent physical conditions
Co-occurrence goes beyond just neurodevelopmental conditions. Neurodivergence very often accompanies physical health differences 2. This isn’t random: in the past decades, there’s been steadily growing biological and genetic evidence for certain conditions to appear together. We now have solid understanding that neurodivergence affects the whole body, not just the brain 1.
This is a major shift in how we think about neurodivergence. The old paradigm treating each condition as separate and isolated is now slowly moving towards a new paradigm based on interconnected parts of a person’s body and brain working together. The growing literature on co-occurrence in neurodevelopmental conditions show how neurodevelopmental differences typically involve multiple areas of functioning rather than isolated symptoms 6.
In practice, if you’re diagnosed with ADHD or autism for example, knowing about co-occurrence means you can recognise related conditions like sleep differences, sensory sensitivities, digestive issues, allergies, immune and dysautonomic conditions. This awareness is especially important because neurodivergent people often experience physical health differences that can affect various other systems of the body. These often get overlooked because the physical co-occurrences often include conditions that are relatively rare in the general population, so they get overlooked as unlikely. However, the differences in probabilities can be staggering: for just one example, over half of neurodivergent adults experience some form of joint hypermobility, compared to only 20% of the general population 2.
3. Mental health conditions co-occurring with neurodivergence
Mental health patterns are an integral part of understanding neurodivergence, especially as for most neurodivergent adults, the road to diagnosing neurodivergent conditions very often leads through diagnoses of anxiety and depressive disorders, which often turn out to have been masking underlying neurodevelopmental differences all along 8.
The numbers are quite telling: over 70% of autistic adults experience at least one additional mental health condition 8.
However, it’s crucial to understand that many mental health challenges aren’t inherently part of being neurodivergent. They often develop as a natural response to navigating a world that isn’t designed for neurodivergent minds and bodies 1.
Neurodivergent people face constant barriers to accessing appropriate support, experience repeated misunderstandings, or struggle to have their needs met in educational, workplace, and healthcare settings. No wonder that anxiety and depression develops as a result. We also have studies showing that more than two thirds of autistic adults have untreated health conditions 1 — it’s no surprise that a chronic lack of appropriate support and understanding can take a severe toll on mental health.
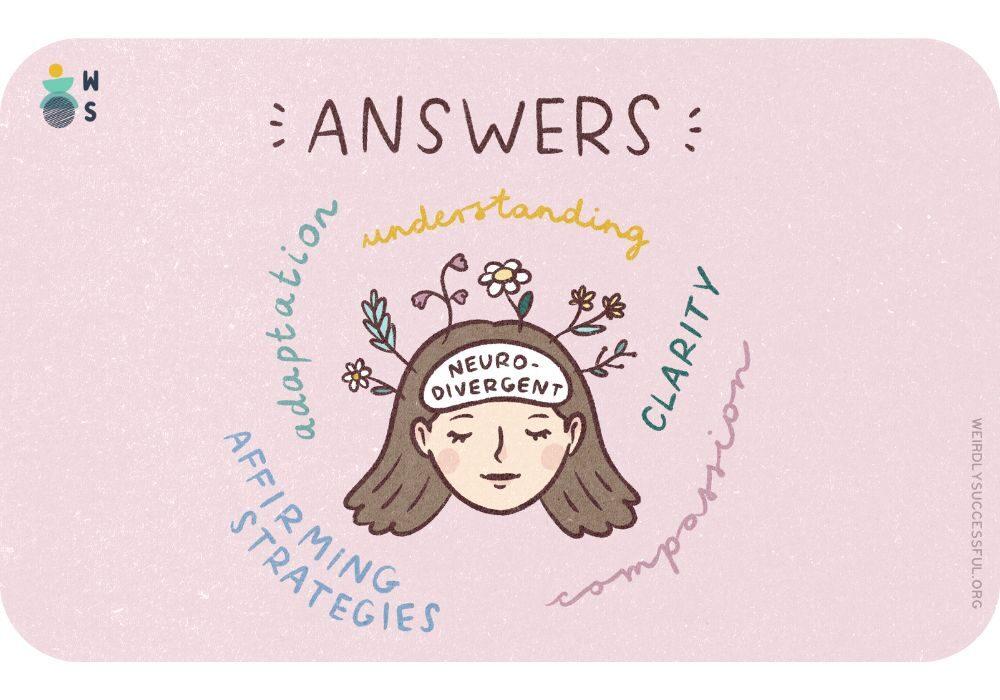
For anyone involved in the care of neurodivergent people, it’s crucial to understanding that markers of anxiety and depression on the surface are often symptoms of the undiagnosed, untreated and unsupported neurodevelopmental conditions that have always been there. Depression and anxiety are therefore not inevitable co-occurring conditions by default, and they’re definitely not the only things to address. In fact, trying to treat anxiety and depression without addressing the underlying neurodivergence can easily lead to worse outcomes.
The bottom line is that exploring symptoms of anxiety and depression as potential results of the lifelong experience of systemic barriers and unmet needs can completely reframe what the right support and treatment looks like for a neurodivergent person.
Why understanding co-occurrence matters
Understanding co-occurrence can be life-changing for neurodivergent people. When you know that different traits and conditions often appear together, it helps make sense of experiences that might have seemed unrelated before. This knowledge is particularly powerful because many healthcare providers aren’t yet familiar with these patterns. One reason for the high percentage of untreated health conditions for neurodivergent people is that symptoms are so often viewed in isolation rather than as part of a larger picture.
For parents of neurodivergent children, understanding co-occurrence can be particularly valuable for early advocacy. When you know that certain conditions often appear together, you can be proactive about watching for signs and ensuring your child gets appropriate support early on, rather than waiting for challenges to become more severe.
For late-identified neurodivergent adults, learning about co-occurrence can help explain lifelong patterns that might have been dismissed or misunderstood. It’s common to have collected various diagnoses over the years without realising they might be connected to underlying neurodevelopmental differences.
Understanding co-occurring conditions isn’t about ‘adding more labels’; it’s about finding better strategies for support and self-advocacy.
Common patterns of co-occurrence
Neurodivergent traits and conditions often cluster together in predictable ways. One of the most well-documented patterns is between ADHD and autism. These two forms of neurodivergence share many underlying genetic and neurological features 7. Learning differences like dyslexia, dyscalculia, and dysgraphia also frequently appear together with both ADHD and autism.
Physical health patterns are equally important to recognise. Many neurodivergent people experience differences in how their autonomic nervous system works (called dysautonomia), which can affect everything from heart rate to digestion. Seemingly random things can fall into place: unusual pain patterns or difficulties with temperature regulation for example can point to underlying joint hypermobility, which leads to the now-known connection between neurodivergence and how the body’s connective tissues work 2.
The gut-brain connection is another crucial pattern. The same systems that affect neurodivergent traits can also influence digestive health and immune system function 34, helping to explain why such a high percentage of neurodivergent people experience digestive differences or food sensitivities – it’s all part of the same interconnected system.
Know your co-occurrences for better support
Understanding co-occurrent conditions can transform how you advocate for yourself in healthcare settings.
Instead of trying to address each symptom or condition separately, you can help healthcare providers see the bigger picture of how different aspects of your health connect. This is particularly important as the standard practice of treating individual conditions in isolation potentially misses important connections that could lead to more effective support.
For example, if you’re seeking help for chronic pain, knowing about the connection between neurodivergence and joint hypermobility might allow you skip years of standard pain treatments and take a more direct route to the connection that would be way down the list of priorities to look into for neurotypical people, but is well-documented for neurodivergent folks. Similarly, understanding how sleep differences and sensory sensitivities often go hand-in-hand with neurodivergence can help you advocate for solutions that address root causes rather than just inadequately managing symptoms with treatments that might work for neurotypical people but won’t for neurodivergent brains.
Parents can use knowledge of co-occurring conditions to advocate for comprehensive assessments and support for their children. For example, if your child has been identified as autistic, understanding co-occurrence might help you recognise and address sensory needs or learning differences earlier, leading to better educational outcomes and reduced stress for your child.
This knowledge is equally valuable in other areas of life. In educational or workplace settings, understanding how different aspects of neurodivergence interact can help you request accommodations that address your full range of needs. For instance, if you know that ADHD and sensory processing differences often co-occur even without an autism diagnosis, you might advocate for both organisational support and sensory-friendly workspace adjustments.
Knowing about co-occurrence extends diagnoses
Remember that you don’t need to have formal diagnoses of co-occurring conditions to benefit from this understanding. Even if your traits don’t meet current diagnostic thresholds or are considered “subclinical,” neurodivergent-friendly approaches can still significantly improve your quality of life 6. Again, this isn’t about collecting labels: knowing the names of things unlock a better understanding of your experiences and needs. This knowledge can help you recognise patterns in your own life and seek appropriate support, even where traditional diagnostic categories don’t perfectly capture your experience. Understanding co-occurrence can help explain why strategies designed for neurodivergent people might work well for you, even if you don’t fully meet diagnostic criteria for any single condition.
Making sense of your journey
Learning about co-occurrence can stir up many emotions. You might feel relieved to finally understand connections between experiences you’ve had your whole life. You might also feel frustrated or angry about not having this information sooner. Both reactions are completely valid. The reality is that our understanding of how neurodivergent traits and conditions connect is still relatively new in the medical world, and this knowledge hasn’t yet made its way into many healthcare settings.
It’s common to look back and realise that signs of co-occurring conditions were there all along, but weren’t recognised because they were viewed in isolation. This is particularly true for people assigned female at birth, who have a much higher rate of going undiagnosed and misdiagnosed.
There’s a difficult balance in working through the mixed feelings of revelation, relief, anger, grief, and so on. But ultimately, there are always practical benefits. Understanding co-occurrence can help explain why certain treatments or approaches might not have worked well in the past – they might have been addressing individual symptoms without recognising the broader patterns.
Remember that discovering these connections isn’t about finding more ‘wrong’ with you – it’s about understanding yourself better and finding more effective ways to support your needs.
Understanding co-occurrence can help you make sense of your past experiences, better advocate for your needs in the present, and make more informed decisions about your support and care in the future.
As for parents, learning about co-occurrence can help you understand both your child’s experiences and, sometimes, your own. Given that neurodivergence runs in families, this knowledge can illuminate patterns across generations, leading to a better understanding and support for everyone involved.
Common co-occurring patterns: A quick reference
Neurodevelopmental Co-occurrences
- ADHD and autism frequently appear together (30-80% of autistic people have ADHD traits, 20-50% of people with ADHD meet autism criteria) 7
- Learning differences (dyslexia, dyscalculia, dysgraphia) often co-occur with both ADHD and autism 6
- Developmental coordination differences (dyspraxia)
- Tourette’s syndrome and tic patterns 2
- Sensory processing differences
Physical Health Patterns
- Joint hypermobility (present in over 50% of neurodivergent adults) 2
- Autonomic nervous system differences (affecting heart rate, temperature regulation, digestion) 2
- Digestive system differences and food sensitivities 34
- Sleep pattern differences
- Chronic pain patterns 2
- Migraine patterns
- Respiratory conditions
Common Systemic Conditions
- POTS (Postural Orthostatic Tachycardia Syndrome)
- EDS (Ehlers-Danlos Syndrome)
- MCAS (Mast Cell Activation Syndrome)
- PMDD (Premenstrual dysphoric disorder)
- Fibromyalgia
- Chronic fatigue patterns
Mental Health Experiences*
- Anxiety
- Depression
- OCD patterns
- Eating differences
- Sleep differences
*Note: Many mental health experiences in neurodivergent people develop as responses to environmental stressors and lack of appropriate support, rather than being inherent to neurodivergence 1.